Search
Better data. Fewer burdens.
Drawing on professional and practice information already entered and verified by providers, the CAQH Directory Management Solution improves health plan directories while reducing redundant, inefficient processes.
Improve Directory Accuracy and Compliance
To enhance accuracy, the CAQH Directory Management Solution applies advanced analytics to data entered, updated and confirmed by physician practices. This multi–layered approach improves data quality, reduces the burden on providers and supports state and federal regulatory compliance.
For delegated groups, administrators are able to centrally manage non-sensitive directory information and make changes to locations, phone numbers and other information once and push it to all providers.
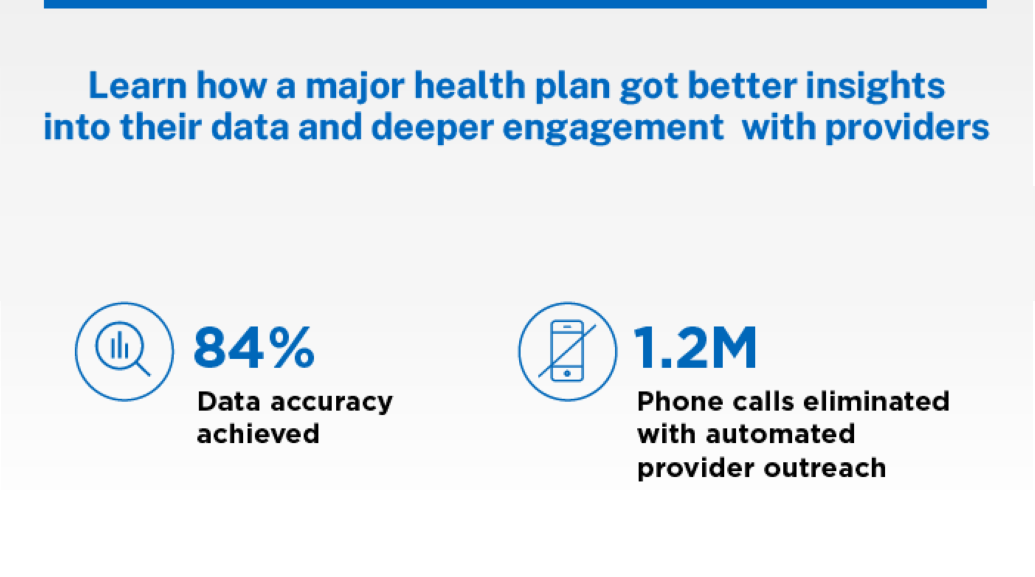
A National Health Plan Achieves 84% Directory Accuracy
One of the nation's largest payers struggling with directory accuracy turned to CAQH for an efficient way to improve data quality without placing additional burdens on providers in its network.